Xpert® SA Nasal Complete
Detection of S. aureus and MRSA in about 65 minutes
Sign in or create a MyCepheid account to add items to cart
Test pack size(s)

10 Tests
GXSACOMP-10
Qty
Unit price
Subtotal
USD
Product is not available for purchase in your region.
Collection devices
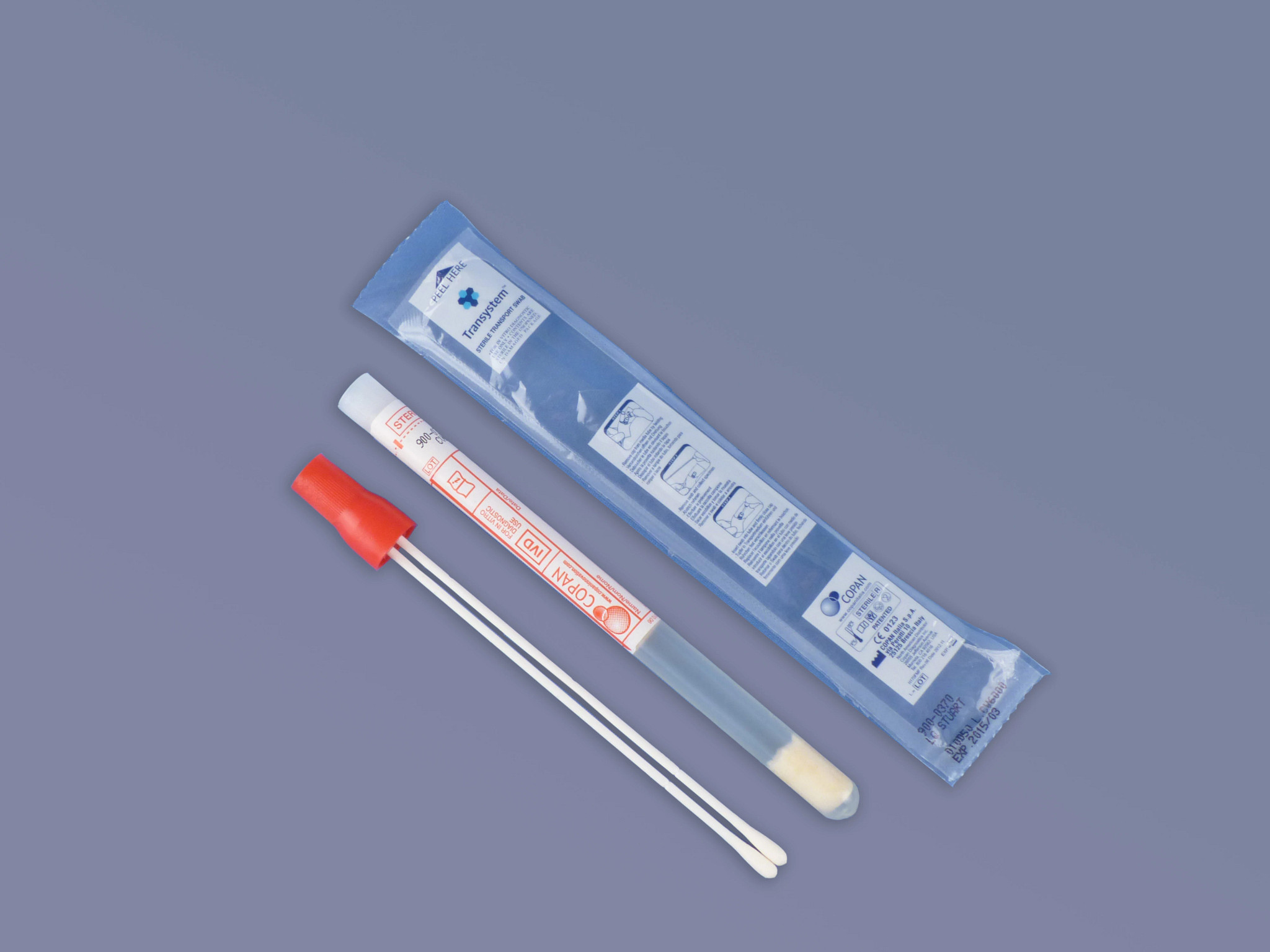
Collection Device (Pack of 50)
900-0370
Qty
Unit price
Subtotal
USD
Product is not available for purchase in your region.
Total
{{currency}}
0
Error adding items to cart. If this error persists, please contact Digital Support
The Need
- Up to 30% of the population is asymptomatically colonized with S. aureus1
- S. aureus colonization can cause life-threatening surgical site infections or other infections in non-surgical patients that increase morbidity, mortality and healthcare costs1
- Perioperative therapeutic strategies vary depending on colonization of MRSA or MSSA2
1 Sakr A, Brégeon F, Mège JL, Rolain JM, Blin O. Staphylococcus aureus Nasal Colonization: An Update on Mechanisms, Epidemiology, Risk Factors, and Subsequent Infections. Front Microbiol. 2018 Oct 8;9:2419. doi: 10.3389/fmicb.2018.02419. PMID: 30349525; PMCID: PMC6186810.
2 Schweizer ML, Chiang H, Septimus E, et al. Association of a Bundled Intervention With Surgical Site Infections Among Patients Undergoing Cardiac, Hip, or Knee Surgery. JAMA. 2015;313(21):2162–2171. doi:10.1001/jama.2015.5387
2 Schweizer ML, Chiang H, Septimus E, et al. Association of a Bundled Intervention With Surgical Site Infections Among Patients Undergoing Cardiac, Hip, or Knee Surgery. JAMA. 2015;313(21):2162–2171. doi:10.1001/jama.2015.5387
The Solution
- Xpert SA Nasal Complete is a qualitative in vitro diagnostic test designed for the detection of S. aureus and methicillin-resistant S. aureus (MRSA) from nasal swabs in patients at risk for nasal colonization
- Identification of S. aureus nasal carriers followed by immediate implementation infection control strategies can signigicantly reduce the risk of hospital acquired S. aureus infections in patients at risk
3 Bode LGM, Kluytmans JAJW, Wertheim HFL, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010;362(1):9-17
* Xpert SA Nasal Complete compared to Reference Culture: (Enriched Blood Agar). Refer to Package Insert 300-8799 Rev. H
* Xpert SA Nasal Complete compared to Reference Culture: (Enriched Blood Agar). Refer to Package Insert 300-8799 Rev. H
The Impact
- Reliable and robust detection of S. aureus and MRSA aids in patient management4
- Rapid implementation of targeted control measures reduces healthcare costs5
- Minutes of hands-on time with results in about 1 hour on a random-access platform
4 Klein EY, Zhu X, Petersen M, Patel EU, Cosgrove SE, Tobian AAR. Methicillin-Resistant and Methicillin-Sensitive Staphylococcus aureus Hospitalizations: National Inpatient Sample, 2016-2019. Open Forum Infect Dis. 2021 Nov 22;9(1):ofab585. doi: 10.1093/ofid/ofab585. PMID: 34988254; PMCID: PMC8715851.
5 Anderson, DJ. Clinical and Financial Outcomes Due to Methicillin Resistant Staphylococcus aureus Surgical Site Infection: A Multi-Center Matched Outcomes Study. PLOS One. 2009 Dec 15. Accessed May 2020. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0008305
5 Anderson, DJ. Clinical and Financial Outcomes Due to Methicillin Resistant Staphylococcus aureus Surgical Site Infection: A Multi-Center Matched Outcomes Study. PLOS One. 2009 Dec 15. Accessed May 2020. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0008305